Precision Diagnostic Services

Upper GI Endoscopy & Colonoscopy
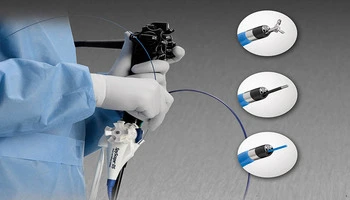
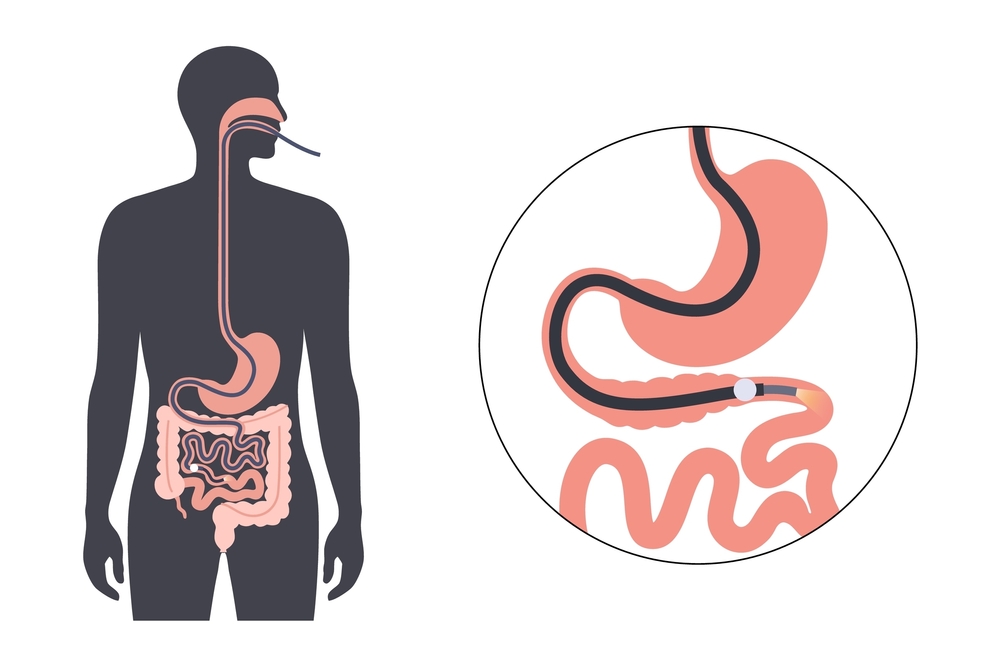
Upper gastrointestinal endoscopy and colonoscopy are cornerstone procedures in modern gastroenterology, allowing direct visualization of the digestive tract for accurate diagnosis and timely treatment. Upper GI endoscopy evaluates the esophagus, stomach, and duodenum, while colonoscopy examines the colon and terminal ileum. These procedures are essential for patients presenting with acidity, heartburn, difficulty swallowing, abdominal pain, anemia, chronic diarrhea, constipation, gastrointestinal bleeding, and unexplained weight loss.
Our center uses high-definition video endoscopes, providing superior image clarity and enhanced mucosal visualization. This allows early detection of subtle inflammatory changes, ulcers, polyps, vascular lesions, and early cancers that may not be visible with standard equipment. Real-time visualization also enables precise biopsy sampling and immediate therapeutic intervention when required.
Colonoscopy plays a vital role in colorectal cancer screening and prevention, as removal of precancerous polyps significantly reduces cancer risk. Both procedures allow therapeutic interventions such as polypectomy, bleeding control, stricture dilatation, and foreign body removal during the same session, often avoiding surgery.
Procedures are performed under monitored sedation to ensure patient comfort and safety, with strict adherence to international infection control and quality standards.
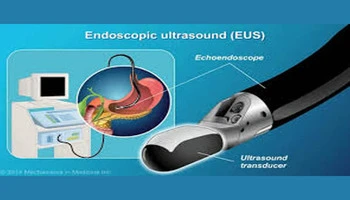
Endoscopic Ultrasonography (EUS)
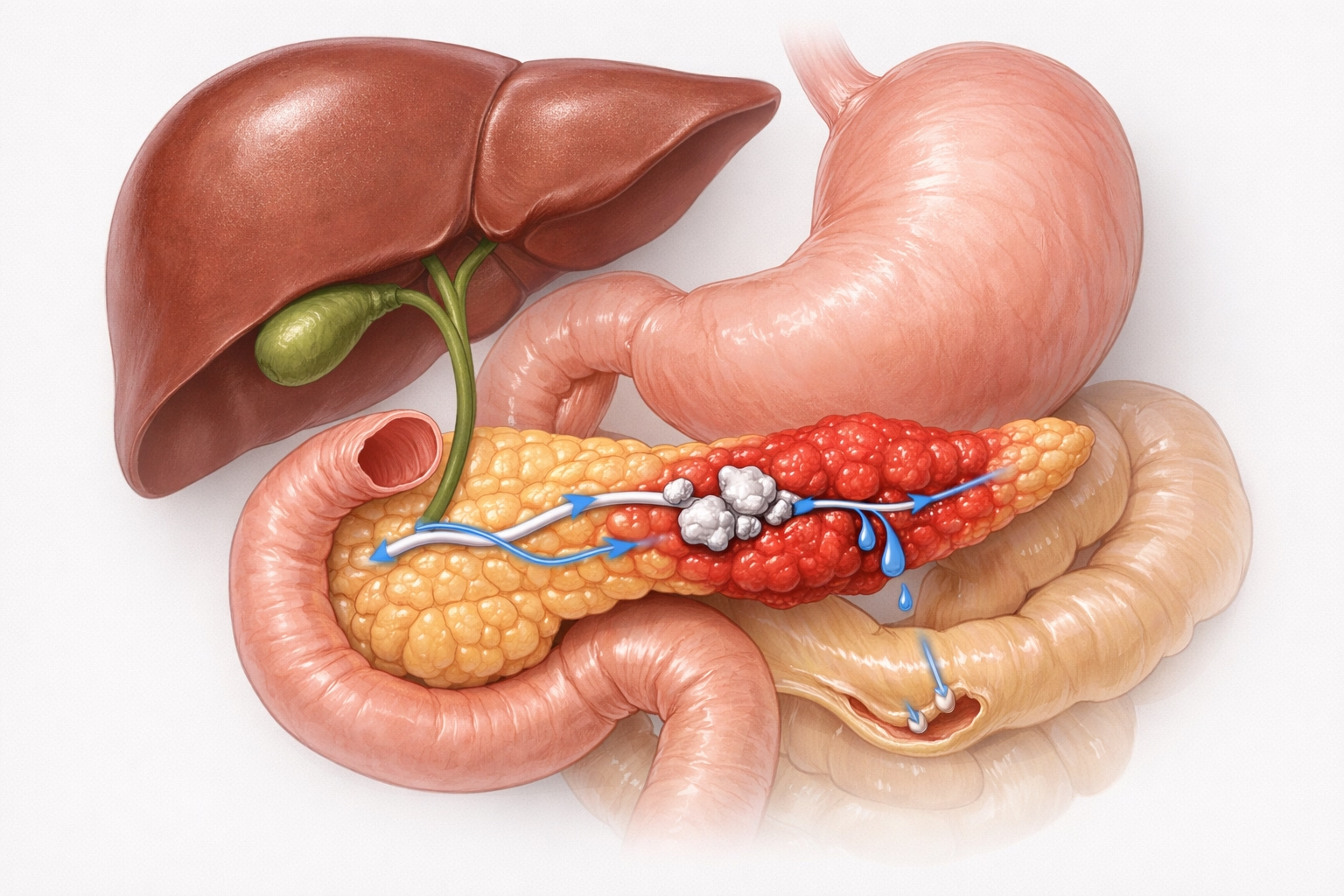
Endoscopic Ultrasonography (EUS) is an advanced imaging modality that combines endoscopy with high-frequency ultrasound to provide detailed visualization of the gastrointestinal wall layers and adjacent organs. It plays a critical role in evaluating pancreatic diseases, biliary disorders, submucosal tumors, lymph nodes, and mediastinal lesions that are difficult to assess with conventional imaging.
EUS offers superior resolution compared to CT and MRI for detecting small pancreatic tumors, cystic lesions, neuroendocrine tumors, and early malignancies. It is also invaluable for staging gastrointestinal cancers and assessing the depth of tumor invasion, guiding appropriate treatment strategies.
Our unit has extensive expertise in therapeutic ERCP, allowing immediate intervention during the same procedure. Common bile duct and pancreatic duct stones are safely removed using baskets.

Fine Needle Aspiration (FNA) and Fine Needle Biopsy (FNB)
Fine Needle Aspiration (FNA) and Fine Needle Biopsy (FNB) allow accurate tissue diagnosis of pancreatic masses, lymph nodes, and deep-seated tumors with minimal risk.

Lumen-Apposing Metal Stents (LAMS)
Lumen-Apposing Metal Stents (LAMS) enable minimally invasive drainage of pancreatic pseudocysts and walled-off necrosis, avoiding open surgery.

EUS-Guided Hepaticogastrostomy
EUS-Guided Hepaticogastrostomy, EUS guided choledochoduodenostomy and EUS guided cholecystogastrostomy provides internal biliary drainage when ERCP fails.
EUS-Guided Celiac Plexus Neurolysis
EUS-Guided Celiac Plexus Neurolysis offers effective pain relief in chronic pancreatitis and pancreatic cancer.
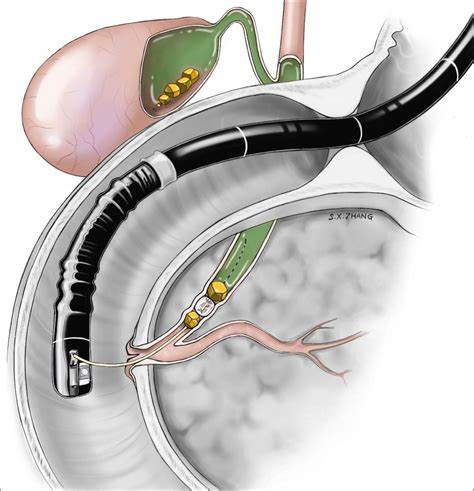
ERCP (Endoscopic Retrograde Cholangiopancreatography)
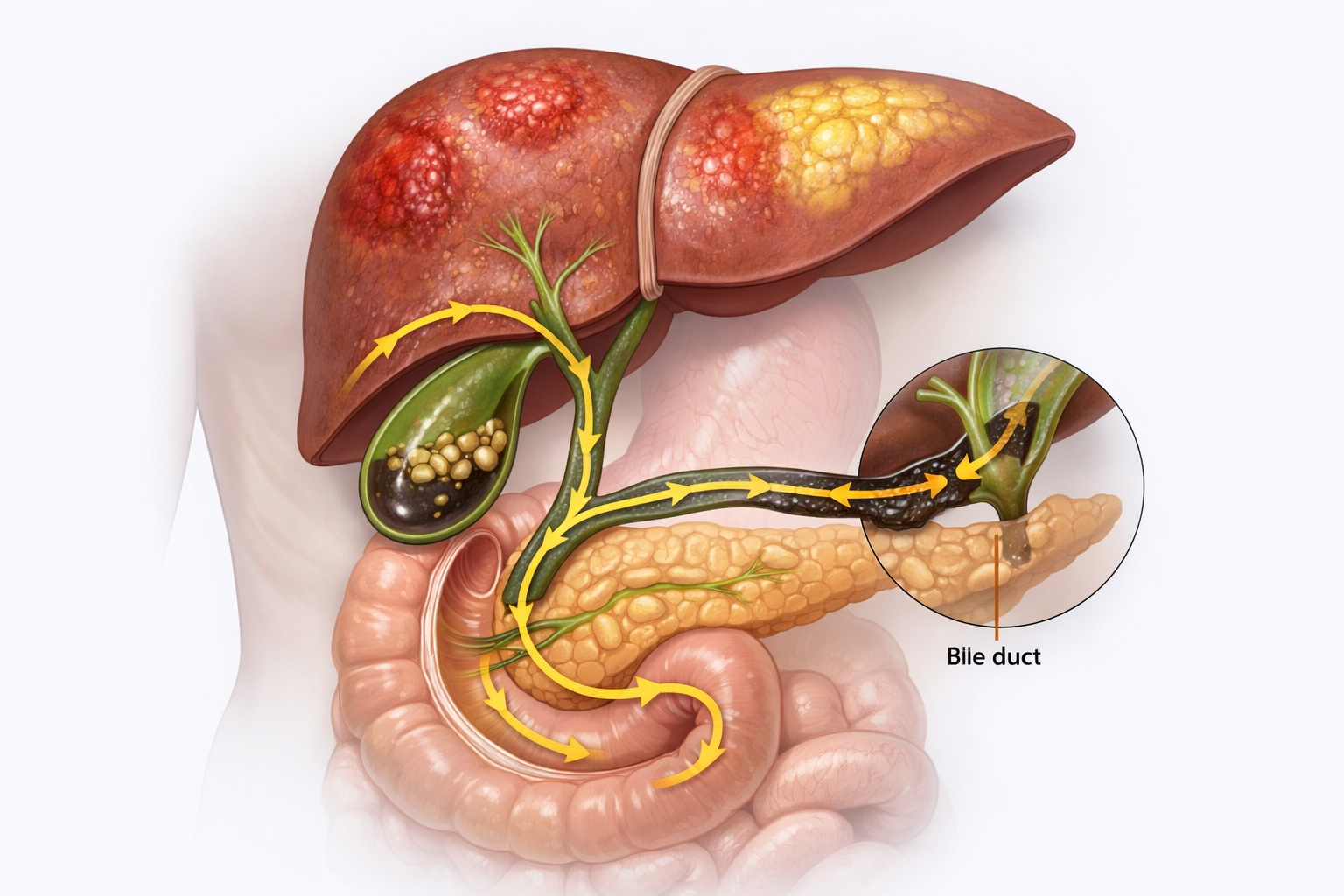
ERCP is a highly specialized endoscopic procedure used for the diagnosis and treatment of biliary and pancreatic duct disorders. It is commonly performed in patients with jaundice, cholangitis, bile duct stones, pancreatic duct strictures, and postoperative bile leaks.
Our unit has extensive expertise in therapeutic ERCP, allowing immediate intervention during the same procedure. Common bile duct and pancreatic duct stones are safely removed using baskets and balloons, relieving obstruction and preventing infection. Plastic and metallic stents are placed to manage benign strictures, malignant obstructions, and cholangiocarcinoma.
Advanced ERCP Techniques:
SpyGlass Cholangioscopy provides direct visualization of the bile ducts, allowing precise assessment of complex strictures, hilar tumors, and indeterminate lesions.
Spy Laser Lithotripsy is used to fragment large or impacted stones that cannot be removed conventionally.
Spy Bite Biopsy enables targeted tissue sampling under direct vision, improving diagnostic accuracy and treatment planning.
Single Balloon Enteroscopy
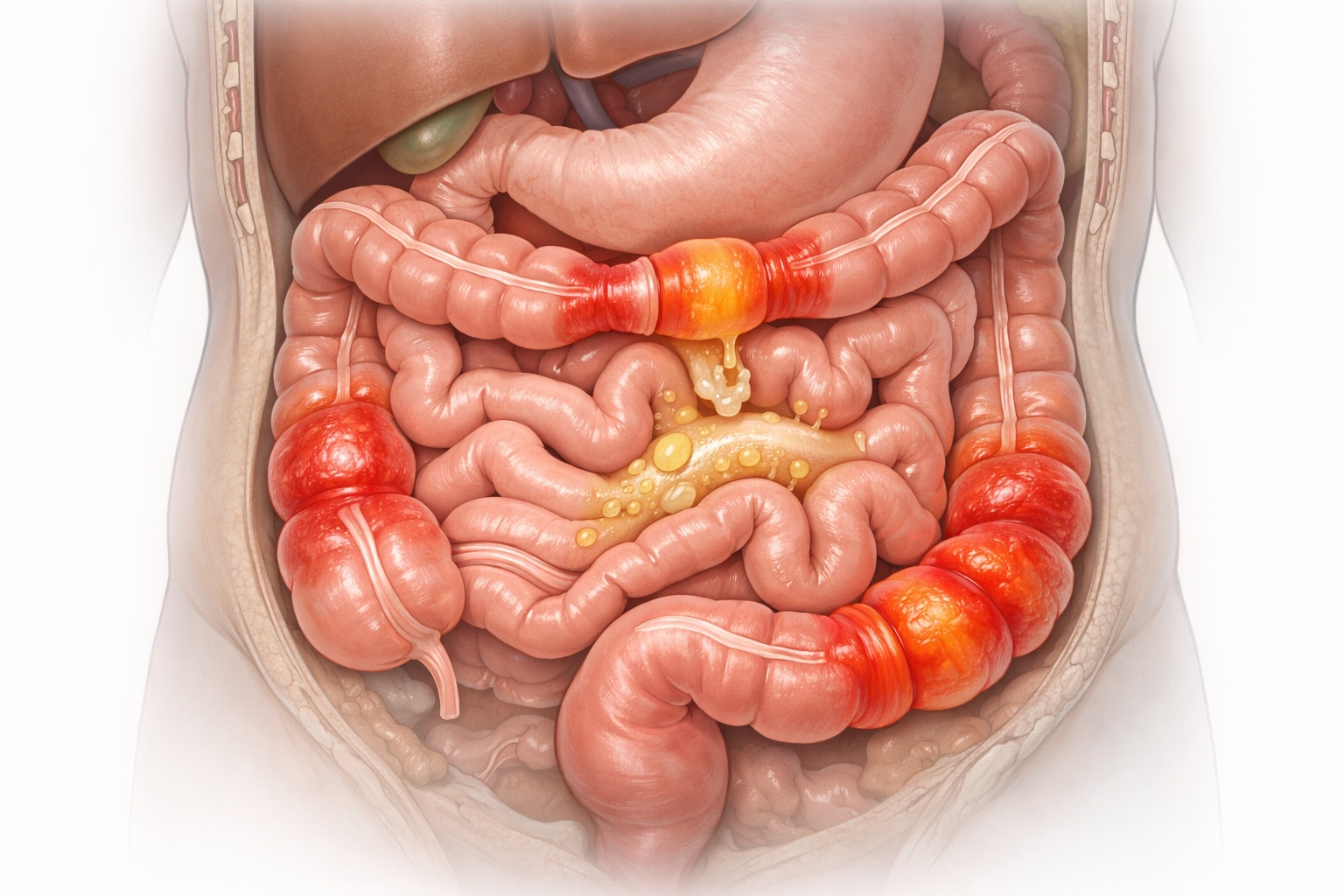
Single balloon enteroscopy is an advanced technique designed to evaluate and treat diseases of the small intestine, an area beyond the reach of routine endoscopy and colonoscopy. It is particularly valuable in patients with obscure gastrointestinal bleeding, unexplained iron-deficiency anemia, small bowel tumors, strictures, polyps, and angioectasias.
Using a balloon-assisted overtube system, the endoscope is gently advanced deep into the small intestine through either the oral or anal route. This allows comprehensive visualization and enables therapeutic interventions during the same session. Procedures such as biopsy, polypectomy, argon plasma coagulation, bleeding control, and stricture dilatation can be performed safely and effectively.
Single balloon enteroscopy significantly reduces the need for repeated investigations and surgical exploration. It plays a crucial role in managing small bowel Crohn's disease, vascular malformations, and inherited polyposis syndromes, offering patients a minimally invasive, organ-preserving treatment option.
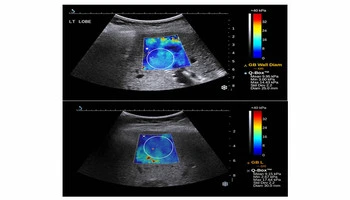
FibroScan & Shear Wave Elastography
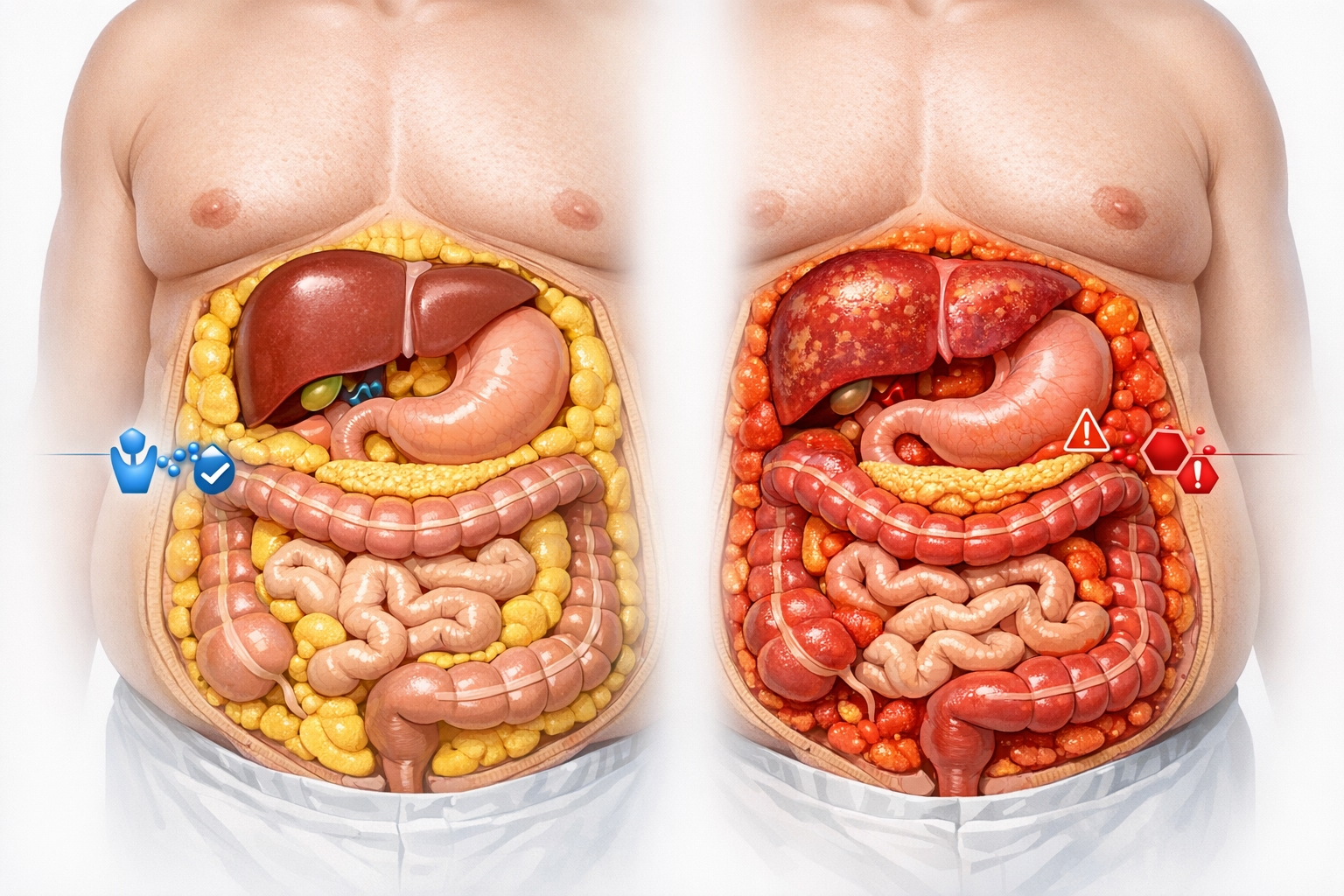
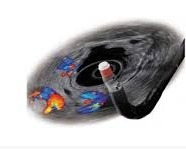
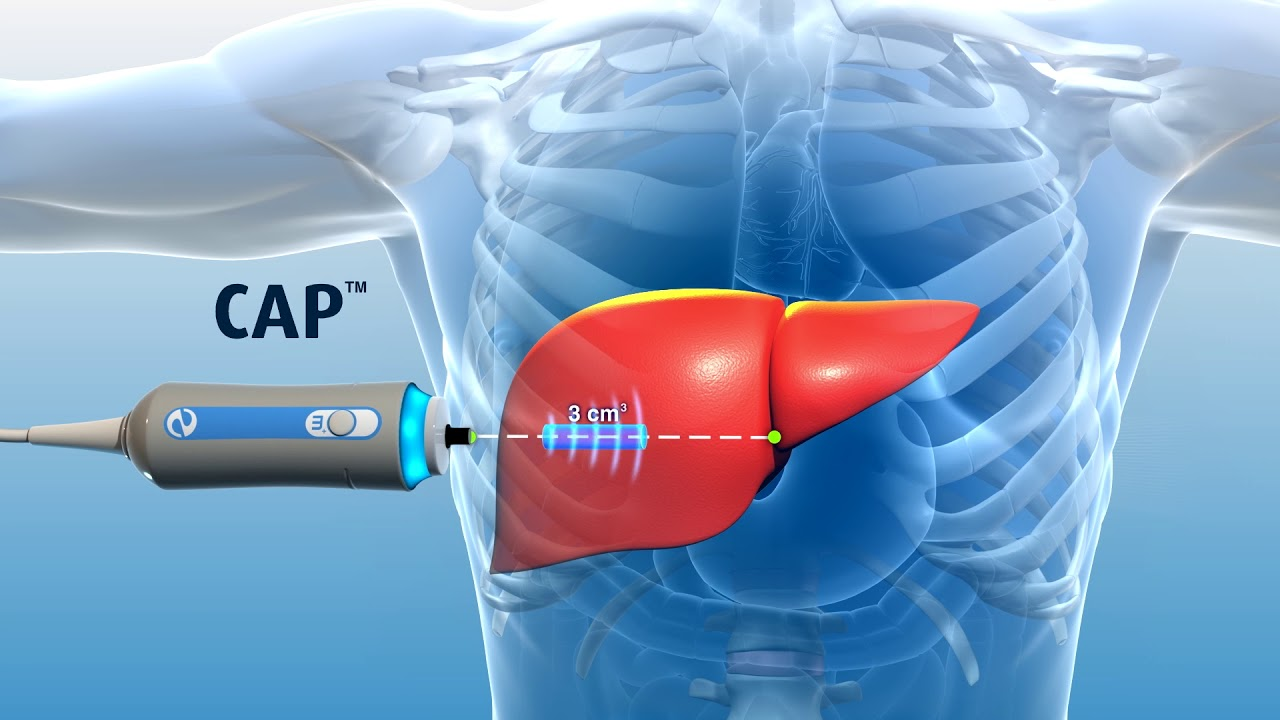
FibroScan and Shear Wave Elastography are advanced, non-invasive imaging techniques used to assess liver stiffness and liver fat content, playing a crucial role in the evaluation and monitoring of chronic liver diseases. These technologies provide accurate quantification of liver fibrosis and steatosis without the need for invasive liver biopsy.
FibroScan measures liver stiffness using transient elastography, helping detect and stage fibrosis in conditions such as fatty liver disease, viral hepatitis, alcoholic liver disease, and autoimmune liver disorders. The Controlled Attenuation Parameter (CAP) component allows precise measurement of liver fat, aiding early diagnosis of metabolic-associated fatty liver disease (MAFLD).
Shear Wave Elastography uses ultrasound-based technology to measure tissue elasticity in real time, offering excellent spatial resolution and the ability to assess focal as well as diffuse liver pathology. It is particularly useful for longitudinal monitoring of disease progression and treatment response.
These tests are painless, quick, and can be repeated safely, making them ideal for screening, prognostication, and follow-up. Early detection of fibrosis allows timely intervention, lifestyle modification, and treatment, significantly reducing the risk of cirrhosis, portal hypertension, and liver-related complications.
Esophageal & Anorectal Manometry, 24-hour pH Monitoring, Electrogastrography
Functional gastrointestinal disorders often present with persistent symptoms despite normal endoscopy findings. Advanced motility and functional testing is essential for accurate diagnosis and targeted management in such cases.
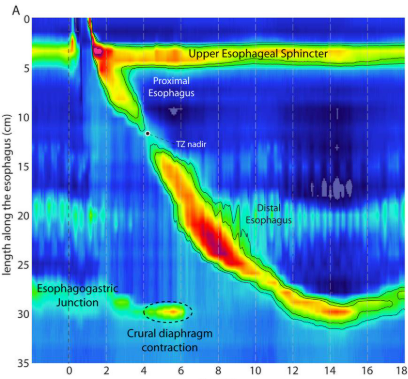
Esophageal Manometry evaluates esophageal muscle contractions and lower esophageal sphincter function, playing a key role in diagnosing achalasia, diffuse esophageal spasm, and ineffective esophageal motility. This test is essential before anti-reflux surgery and POEM procedures.
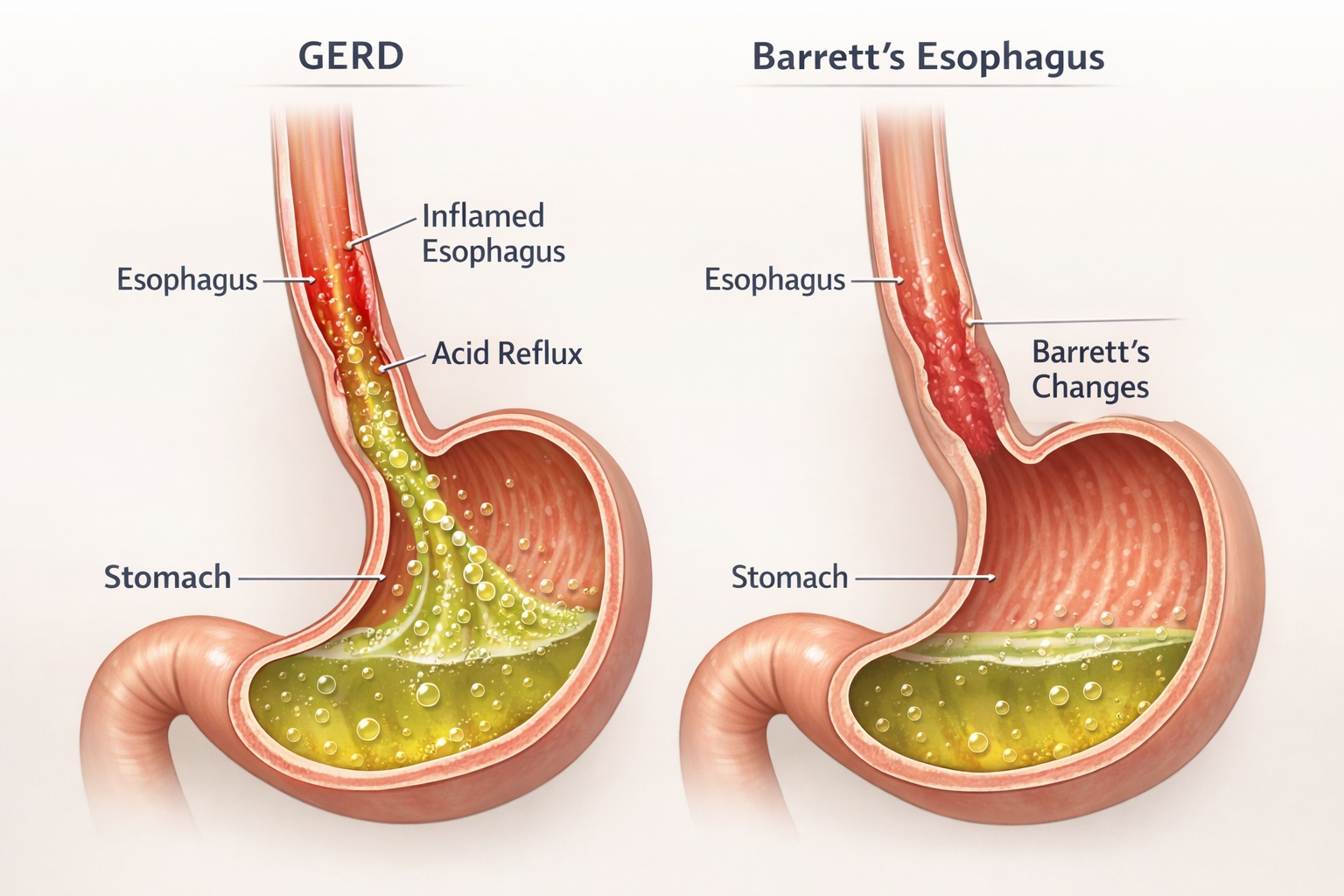
24-hour pH Monitoring accurately measures acid exposure in the esophagus, confirming gastroesophageal reflux disease (GERD) and correlating symptoms with reflux episodes. It helps differentiate true acid reflux from functional heartburn.
Anorectal Manometry assesses rectal sensation, anal sphincter pressures, and coordination during defecation, aiding diagnosis of chronic constipation, dyssynergic defecation, and fecal incontinence.
Electrogastrography evaluates gastric electrical activity, providing insights into gastric motility disorders such as gastroparesis. These tests enable personalized treatment strategies, improving long-term symptom control and quality of life.

Breath Tests
Breath tests provide a simple, non-invasive method to diagnose specific gastrointestinal disorders related to infections and carbohydrate malabsorption. These tests are safe, painless, and highly reliable when performed under standardized protocols.
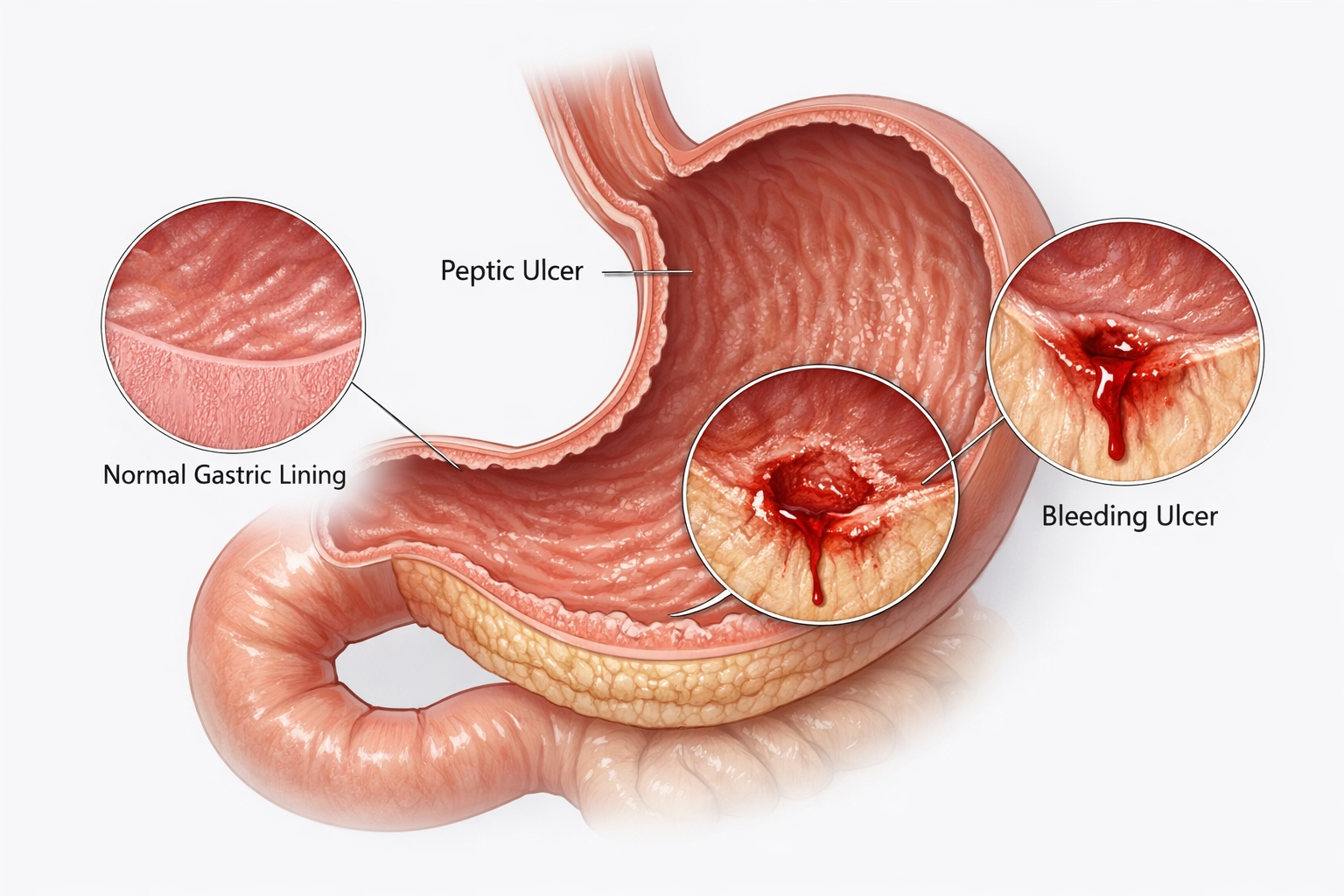
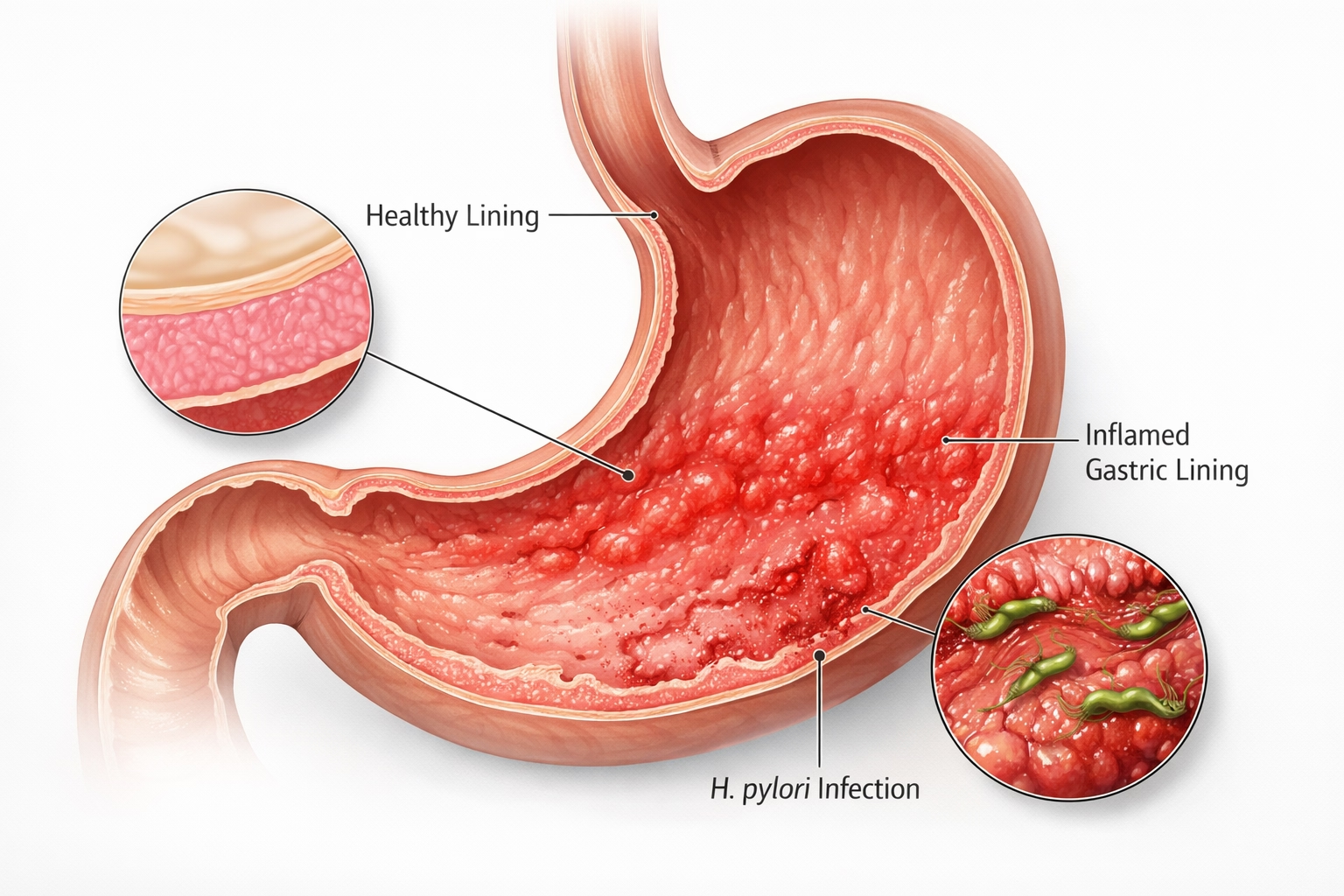
The Urea Breath Test is considered the gold standard non-invasive test for detecting Helicobacter pylori infection. Accurate diagnosis and post-treatment confirmation of eradication are essential in patients with peptic ulcer disease, dyspepsia, and gastric cancer risk.
The Lactose Breath Test is used to diagnose lactose intolerance by measuring hydrogen or methane production after lactose ingestion. It helps differentiate lactose intolerance from other causes of bloating, abdominal pain, and diarrhea.
Breath testing also aids in diagnosing Small Intestinal Bacterial Overgrowth (SIBO), which can cause chronic bloating, malabsorption, and unexplained gastrointestinal symptoms. Accurate diagnosis allows targeted antibiotic therapy and dietary modification, preventing unnecessary investigations and prolonged symptoms.
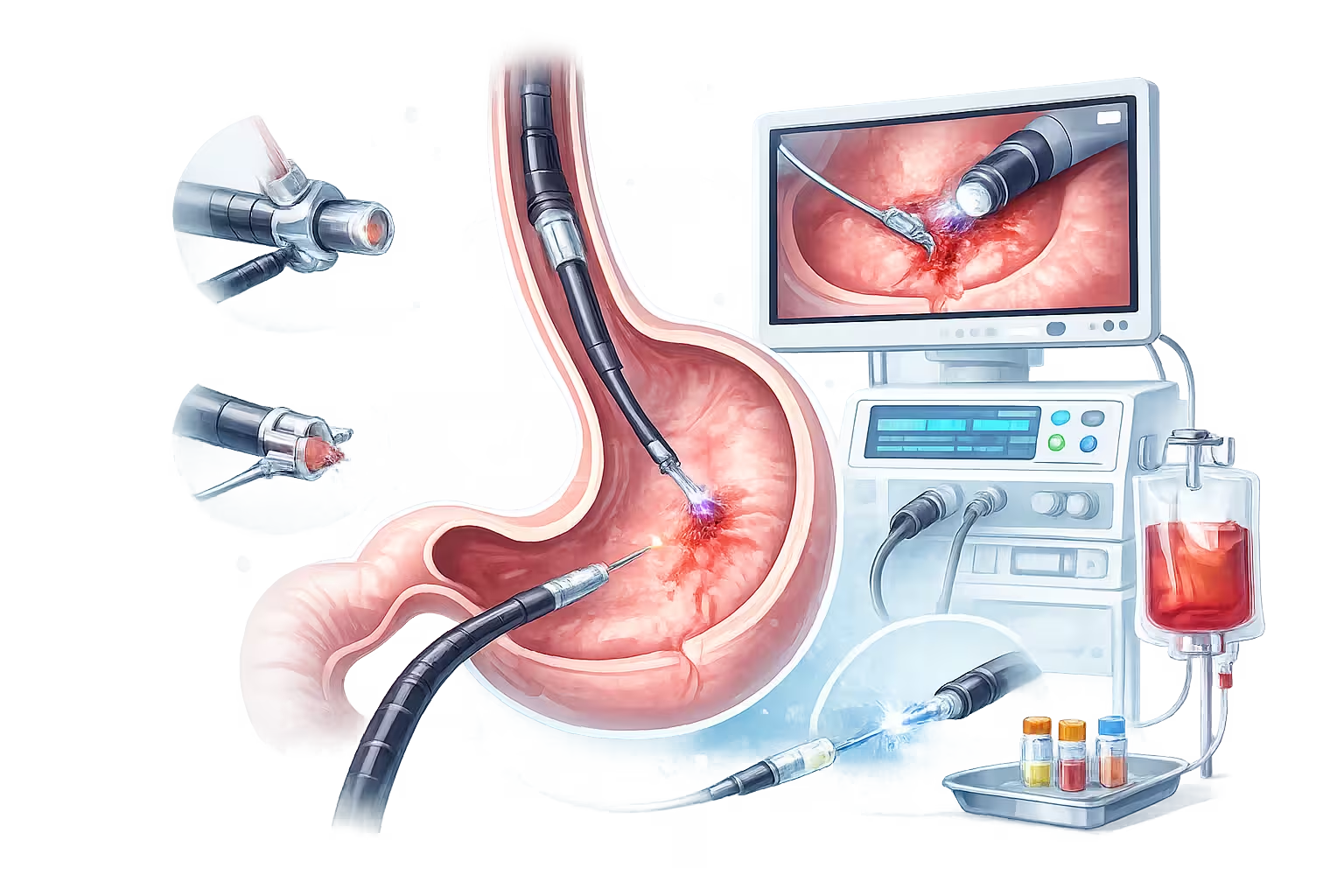
Gastrointestinal Bleeding Management
Endoscopic management of gastrointestinal bleeding is a life-saving intervention that allows rapid diagnosis and immediate treatment. Our center offers comprehensive endoscopic bleeding control for both upper and lower GI bleeding.
Peptic Ulcer Bleeding is managed using advanced techniques such as hemoclipping, injection therapy, and Ovesco clip application for large or refractory ulcers.
Variceal Bleeding is treated using endoscopic band ligation for esophageal varices and glue injection or stenting for fundal varices. Collagen spray is used as an adjunct for diffuse bleeding.
Argon Plasma Coagulation (APC) is an effective, non-contact method for treating angioectasias, portal hypertensive gastropathy, and radiation-induced bleeding.
Prompt endoscopic intervention reduces mortality, blood transfusion requirements, and hospital stay, ensuring optimal outcomes even in high-risk patients.

Biofeedback Therapy for Pelvic Floor & Defecation Disorders
Biofeedback therapy is a highly effective, non-invasive treatment offered to patients diagnosed with pelvic floor dysfunction after anorectal manometry testing. Many individuals with chronic constipation, difficulty in passing stools, or a sensation of incomplete evacuation have a condition known as dyssynergic defecation , where the pelvic floor muscles fail to relax appropriately during bowel movements.
Biofeedback works by retraining the muscles and nerves involved in defecation using real-time visual and sensory feedback. During the therapy session, small sensors are placed to monitor anal sphincter pressures and muscle coordination. Patients are guided by a trained therapist to learn correct muscle relaxation, abdominal push techniques, and coordinated bowel movements.
This therapy is completely safe, does not involve medications or surgery, and has been shown to provide long-term symptom relief in a majority of patients. Biofeedback is especially beneficial for individuals who have not responded adequately to laxatives or dietary measures.
Regular sessions help improve bowel habits, reduce dependence on medications, prevent complications such as fissures and hemorrhoids, and significantly enhance quality of life. When combined with dietary counseling and lifestyle modification, biofeedback therapy offers a durable and evidence-based solution for functional anorectal disorders.
Foreign Body & Gastrointestinal Stricture Management
Foreign body ingestion and gastrointestinal strictures can cause significant discomfort, obstruction, and serious complications if not treated promptly. Advanced endoscopic techniques allow safe, minimally invasive management without the need for open surgery in most cases.
Foreign body retrieval is commonly required in children and adults who accidentally ingest coins, batteries, bones, dentures, or food boluses. Using specialized endoscopic accessories such as retrieval forceps, snares, and baskets, objects can be removed safely under direct vision, reducing the risk of perforation or infection.
Esophageal strictures, often caused by chronic acid reflux, radiation, surgery, or caustic ingestion, are treated using CRE balloon dilatation. This controlled and graded dilation relieves dysphagia and restores normal swallowing.
For patients with advanced gastrointestinal cancers, metallic stenting provides effective palliation by relieving obstruction and allowing oral intake. Pyloric balloon dilatation and enteral stenting are used in gastric outlet obstruction to improve nutrition and quality of life.
These endoscopic interventions are safe, effective, and significantly reduce hospital stay while improving patient comfort and outcomes.

Tumor & Lesion Management
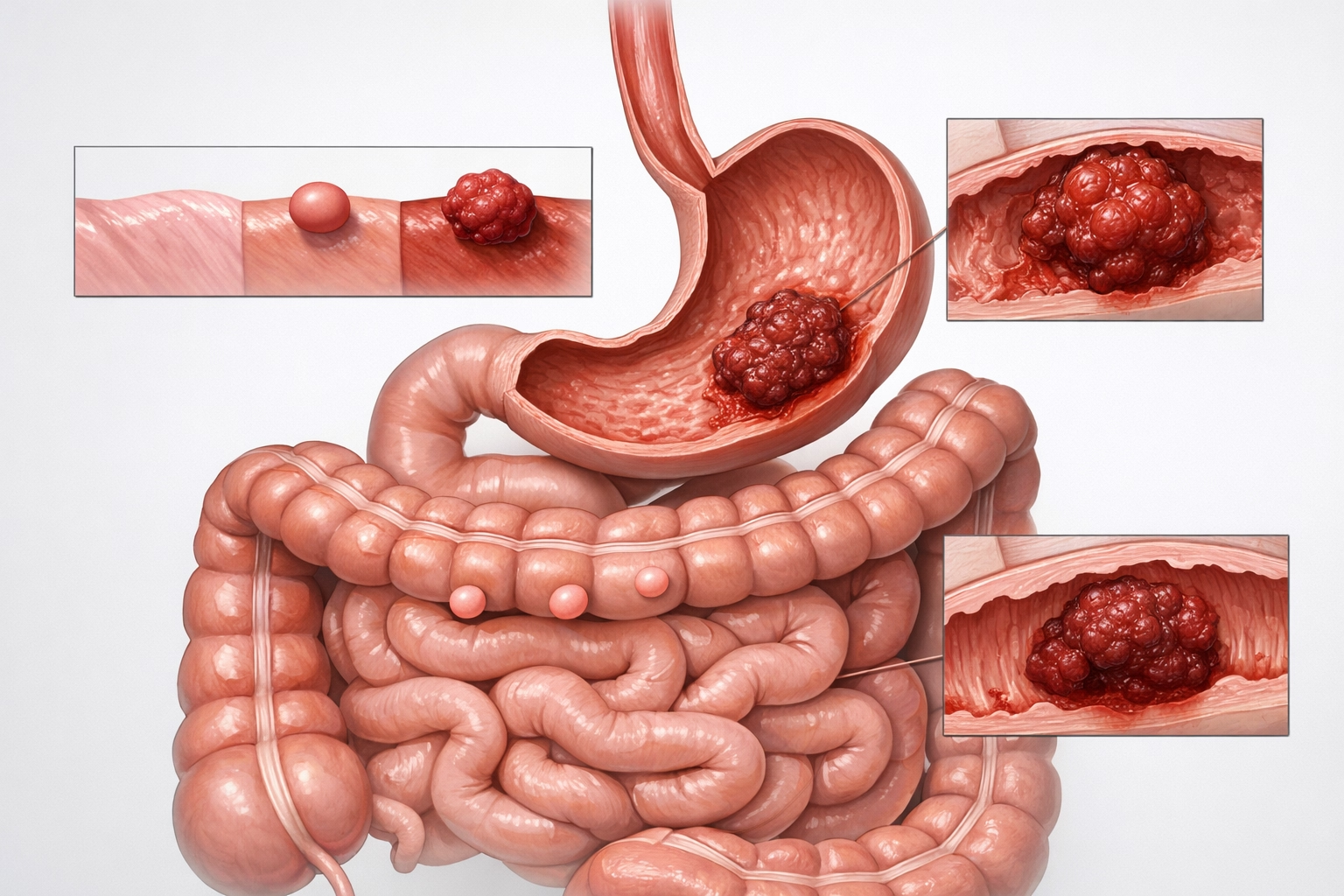
Early detection and minimally invasive treatment of gastrointestinal tumors and precancerous lesions are critical in preventing cancer progression and avoiding major surgery. Advanced endoscopic imaging and therapeutic techniques play a central role in modern GI oncology.
Narrow Band Imaging (NBI) enhances mucosal and vascular patterns, allowing early detection of subtle precancerous and cancerous lesions in the esophagus, stomach, and colon. This enables targeted biopsies and accurate surveillance.
Radiofrequency Ablation (RFA) is an established therapy for Barrett's esophagus with dysplasia, effectively eradicating abnormal mucosa and reducing the risk of progression to esophageal cancer.
Polypectomy and endolooping are routinely performed for safe removal of colorectal and gastric polyps, preventing malignant transformation. Larger or high-risk polyps can be managed endoscopically without surgery.
Early intervention using these techniques leads to excellent long-term outcomes, reduces cancer-related mortality, and allows organ preservation with minimal recovery time.

PEG & NJ Tube Insertions for Enteral Nutrition
Patients who are unable to consume adequate nutrition orally due to neurological disorders, malignancy, or prolonged critical illness benefit greatly from enteral feeding access. Percutaneous Endoscopic Gastrostomy (PEG) and Nasojejunal (NJ) tube placements provide safe and effective long-term nutritional support.
PEG tube insertion is performed endoscopically and allows direct feeding into the stomach. It is ideal for patients with stroke, neurodegenerative disorders, head and neck cancers, and chronic swallowing difficulties.
NJ tube placement delivers nutrition directly into the jejunum and is preferred in patients with severe reflux, pancreatitis, or gastric outlet obstruction. Endoscopic placement ensures accurate positioning and reduces complications.
These procedures are minimally invasive, well tolerated, and significantly improve nutritional status, wound healing, immunity, and overall recovery. Proper nutritional support plays a vital role in improving survival and quality of life in chronically ill patients.
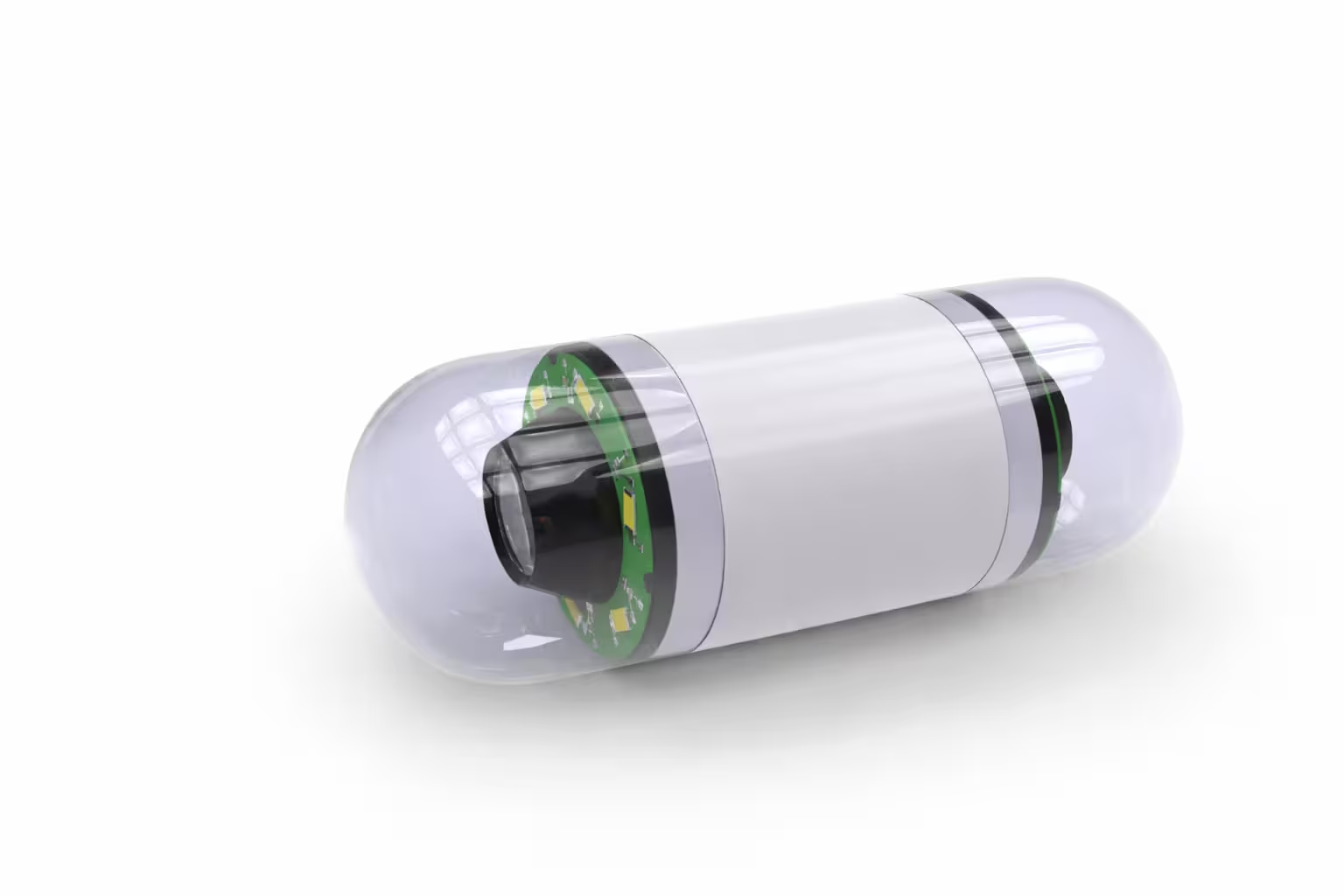
Capsule Endoscopy
Capsule endoscopy is a revolutionary, non-invasive technique that allows visualization of the entire small intestine, an area not easily accessible by conventional endoscopy or colonoscopy.
The patient swallows a pill-sized capsule containing a miniature camera, light source, and transmitter. As it travels naturally through the gastrointestinal tract, it captures thousands of high-resolution images, which are recorded and analyzed by the gastroenterologist.
Capsule endoscopy is particularly useful in evaluating obscure gastrointestinal bleeding, unexplained anemia, suspected Crohn's disease, small bowel tumors, polyps, and angioectasias. It is also helpful in assessing malabsorption syndromes and chronic abdominal pain when other tests are inconclusive.
The procedure is painless, requires no sedation, and allows patients to continue most daily activities. Capsule endoscopy has significantly improved diagnostic accuracy for small bowel diseases and guides further targeted therapy when needed.
Third Space Endoscopy
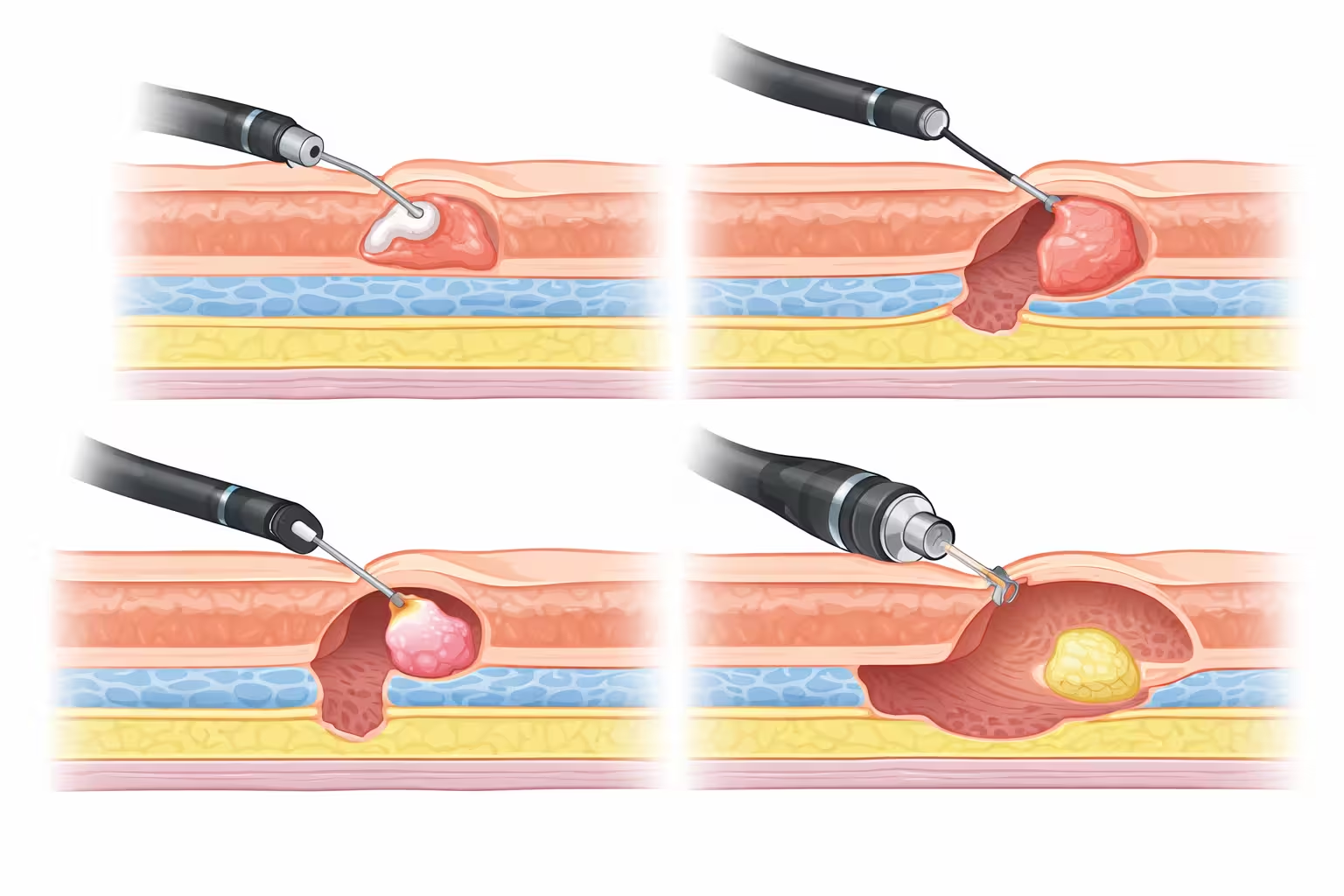
Third space endoscopy represents a major advancement in minimally invasive gastrointestinal surgery, allowing complex lesions and motility disorders to be treated entirely through the endoscope without external incisions. These procedures target the "submucosal or third space" layer of the gastrointestinal tract, enabling precise and organ-preserving therapy.
Endoscopic Mucosal Resection (EMR) is used for removal of superficial precancerous and early cancerous lesions confined to the mucosa. It is a safe, effective alternative to surgery for selected patients.
Endoscopic Submucosal Dissection (ESD) allows en-bloc resection of larger or deeper lesions, ensuring complete removal with clear margins. ESD provides curative treatment for early gastrointestinal cancers while preserving normal anatomy.
Full Thickness Resection Device (FTRD) enables removal of difficult lesions involving deeper layers of the bowel wall, especially in previously operated or fibrotic areas.
Submucosal Tunneling Endoscopic Resection (STER) is used for removal of subepithelial tumors such as gastrointestinal stromal tumors while maintaining mucosal integrity.
These advanced procedures reduce hospital stay, avoid major surgery, and provide excellent long-term outcomes.

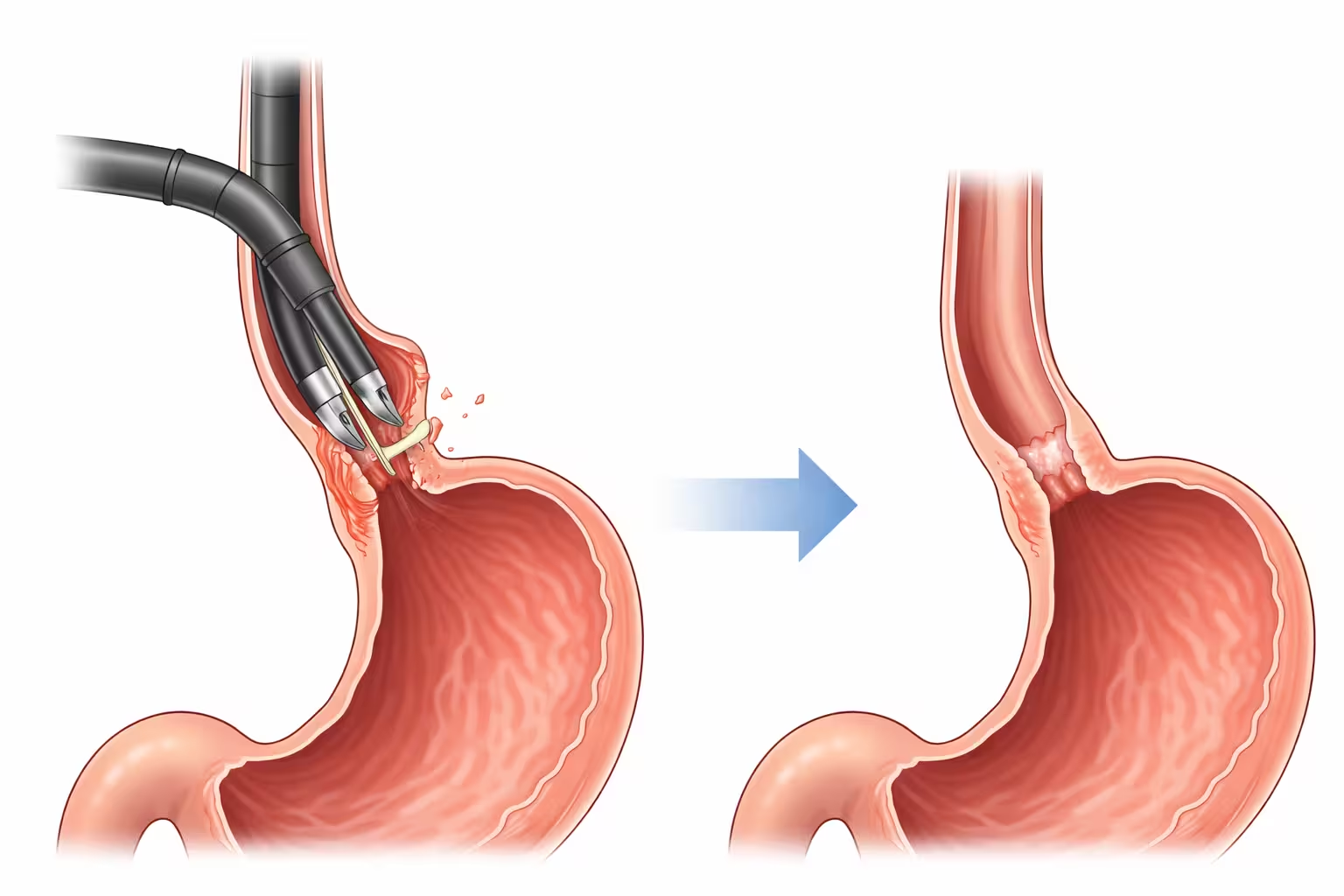
POEM (Peroral Endoscopic Myotomy) for Achalasia
POEM is a state-of-the-art endoscopic procedure used to treat achalasia cardia and other esophageal motility disorders. Achalasia occurs when the lower esophageal sphincter fails to relax, leading to difficulty swallowing, chest pain, regurgitation, and weight loss.
During POEM, a tunnel is created within the esophageal wall using an endoscope, allowing precise division of the abnormal muscle fibers responsible for obstruction. This restores normal food passage into the stomach without any external incision.
POEM offers excellent symptom relief, even in patients who have failed previous treatments such as balloon dilation or surgery. The procedure is safe, minimally invasive, and associated with rapid recovery and short hospital stay.
POEM has revolutionized the management of achalasia by providing durable, long-term results with minimal discomfort. It is also effective for spastic esophageal disorders such as diffuse esophageal spasm and jackhammer esophagus.
ARMS (Anti-Reflux Mucosectomy)
ARMS, or Anti-Reflux Mucosectomy, is an innovative endoscopic treatment for patients with gastroesophageal reflux disease (GERD) who do not respond adequately to medications. Unlike traditional anti-reflux surgery, ARMS is performed entirely through an endoscope without external cuts.
The procedure involves controlled removal of mucosa at the gastroesophageal junction, leading to scarring and tightening of the anti-reflux barrier. This enhances the natural valve mechanism and significantly reduces acid reflux.
ARMS is particularly useful for patients with early GERD, small hiatal hernias, or persistent symptoms despite optimal medical therapy. It preserves normal anatomy while offering durable symptom control.
Patients experience improvement in heartburn, regurgitation, and dependence on acid-suppressing medications. Recovery is quick, and complications are minimal when performed by experienced endoscopists.

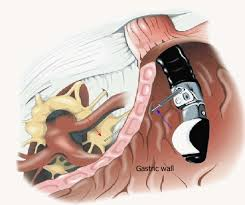
EUS-Guided Cholecystogastrostomy & Choledochoduodenostomy
EUS-guided biliary and gallbladder drainage procedures are advanced alternatives for patients in whom conventional ERCP is not feasible. These minimally invasive techniques provide internal drainage without the need for surgery or external tubes.
EUS-guided cholecystogastrostomy involves creating a connection between the gallbladder and stomach using a lumen-apposing metal stent (LAMS). It is especially beneficial for high-risk surgical patients with acute cholecystitis.
EUS-guided choledochoduodenostomy establishes drainage between the bile duct and duodenum, providing effective relief from biliary obstruction due to stones or malignancy.
These procedures offer rapid symptom relief, lower complication rates, and improved patient comfort compared to percutaneous drainage. They represent cutting-edge endoscopic care for complex biliary disorders.
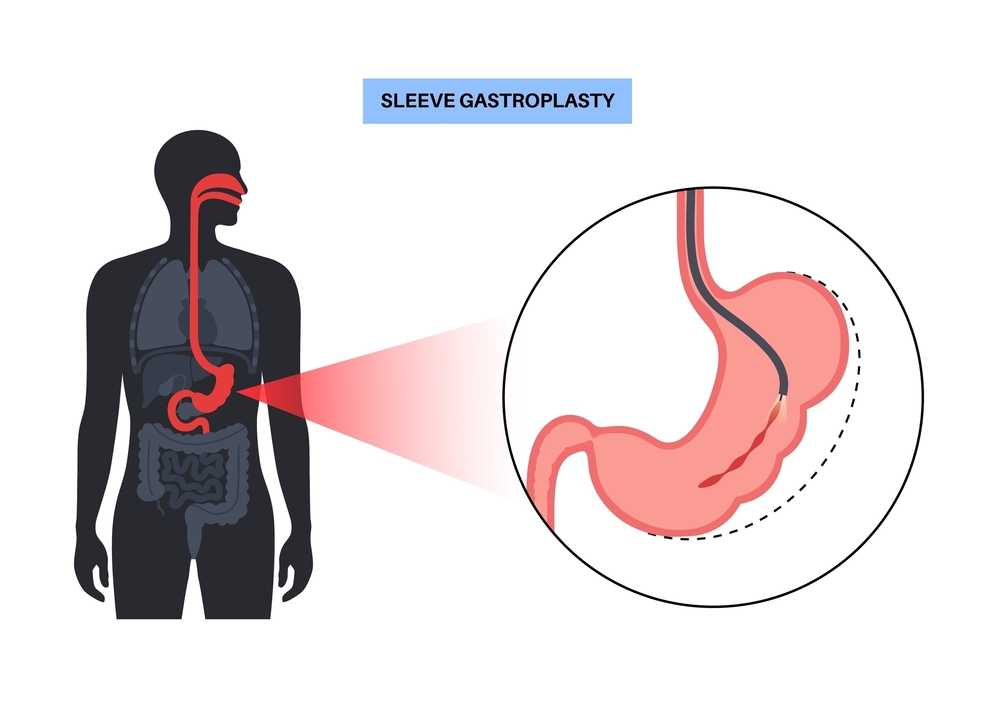
Obesity & Endobariatrics
Endobariatrics offers minimally invasive, endoscopic solutions for weight loss and metabolic improvement, providing effective alternatives to bariatric surgery.
Endoscopic Sleeve Gastroplasty (ESG) reduces stomach volume using endoscopic suturing, promoting early satiety and sustained weight loss. It is ideal for patients seeking a non-surgical option with rapid recovery.
Spatz Balloon is an adjustable intragastric balloon that allows volume modification based on patient tolerance and weight loss response.
Allurion Balloon is unique in that it can be swallowed without endoscopy or anesthesia and naturally passes out of the body after treatment. It supports significant weight loss with minimal downtime.
Endobariatric procedures improve obesity-related conditions such as fatty liver disease, diabetes, hypertension, and GERD, under expert medical supervision.